
51
19–22 APRIL, 2017, BARCELONA, SPAIN
08:41–08:44
S4-5 (PP)
HOW DID OUR TREATMENTS BEFORE AND AFTER EAU/
ESPU VUR RISK GROUPING SYSTEM AFFECT OUR EARLY
SUCCESS RATES?
Eda TOKAT
1
, Serhat GUROCAK
1
, Iyimser URE
2
, Cenk ACAR
3
, Zafer SINIK
4
and Ozgur TAN
1
1) Gazi University School of Medicine, Department of Urology, Section of Paediatric Urology, Ankara, TURKEY -
2) Eskisehir Osmangazi University School Of Medicine, Department of Urology, Section of Paediatric Urology, EskISehIr,
TURKEY - 3) ERYAMAN HOSPITAL, Department of Urology, Ankara, TURKEY - 4) ODAK HOSPITAL, Department
of Urology, Denizli, TURKEY
PURPOSE
To compare the early clinical results of treatments performed before and after EAU/ESPU VUR
classification due to vesicoureteral reflux.
MATERIAL AND METHODS
296 out of 346 renal units with regular clinical follow-up data who were treated due to VUR between
2009-2016 were retrospectively reviewed by dividing our patients into two groups as before and
after 2013. Preoperative clinical parameters as grade and laterality of reflux, presence of renal
scar, initial and follow-up treatments , findings of medical treatment and surgical procedures were
analysed. Clinical failure was identified as; surgery for nonresponsive cases to medication, sympto-
matic urinary tract infection after surgery and new renal scar in postoperative DMSA.
RESULTS
Mean age and follow-up length were 75(6-132)months and 27,2(6-78)months respectively. In the
low risk group,clinical success rates of medical and surgical treatments before the risk classifica-
tion were %38,5 and %87,9 respectively. (Table). We determined that VUR risk grouping does not
change clinical success significantly in all groups (p0.062; p:0,063; p:0,459, respectively)
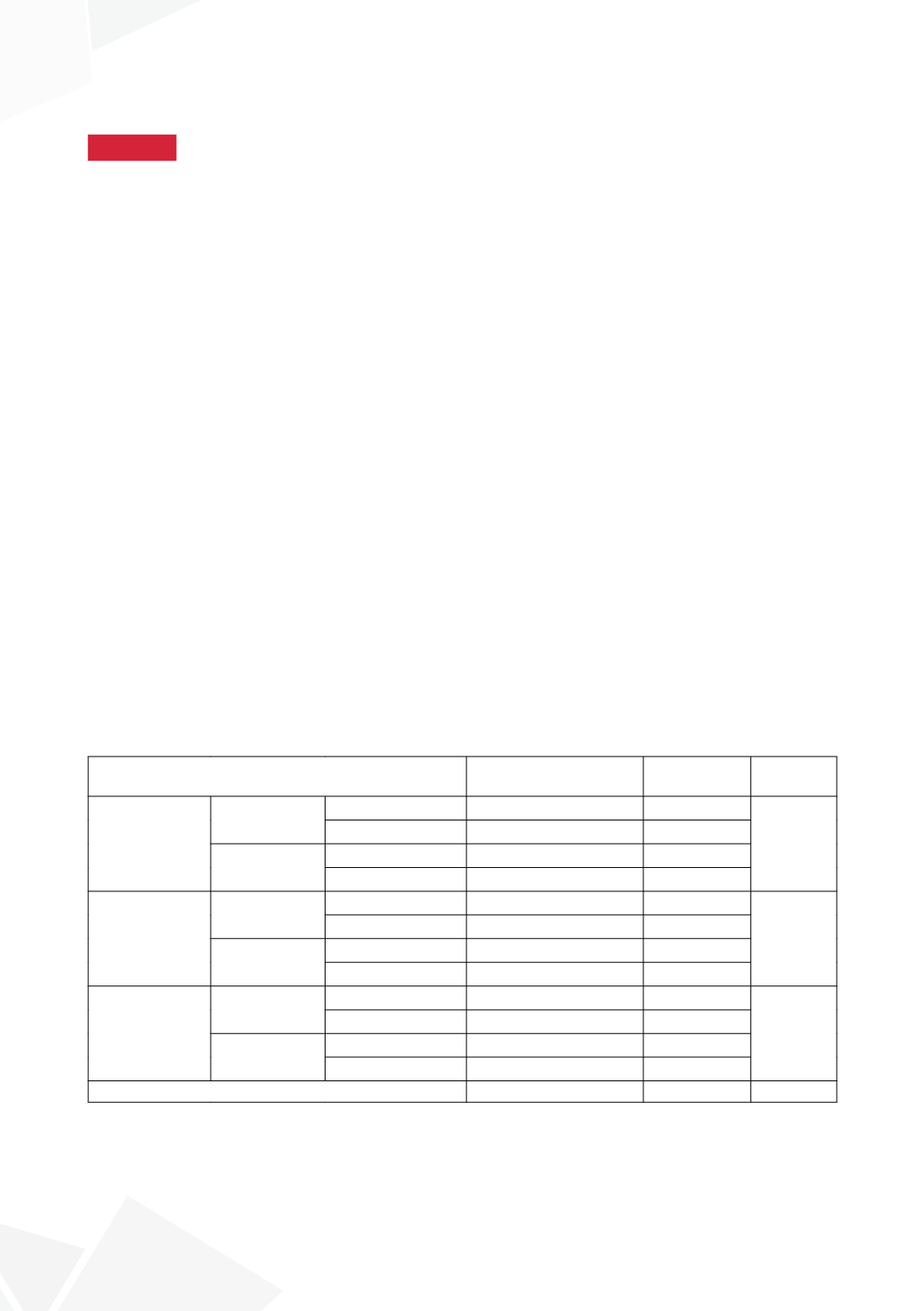
EAU/ESPU VUR classification
Medical treatment
(%)
Surgical
treatment (%)
p value
Low risk
Before 2013 Successful
5(38,5)
29(87,9)
0,062
Unsuccessful
8(61,5)
4(12,1)
After 2013
Successful
7 (36,8)
6 (100)
Unsuccessful
12 (63,2)
0
Moderate risk Before 2013 Successful
16(30,8)
83(90,2)
0,063
Unsuccessful
36(69,2)
9(9,8)
After 2013
Successful
2(16,7)
18(69,2)
Unsuccessful
10(83,3)
8(30,8)
High risk
Before 2013 Successful
1(10)
14(56)
0,459
Unsuccessful
16(94,1)
11(44)
After 2013
Successful
0
1 (100)
Unsuccessful
0
0
Total
113(38,2)
183(61,8)
CONCLUSIONS
Despite the fact that EAU/ESPU VUR risk classification changed our current practice in terms
of initial treatment method, this different approach did not seem to affect early clinical success
positively. There is still an absolute need for studies with larger sample size and long-term follow-up
to reach more reliable results.









