Introduction
Incontinence has a significant impact on the daily functioning of both the child and the family and is increasingly recognized as a problem in children. For these children, urotherapy offers a solution. Urotherapy is a standard treatment for children with bladder and lower urinary tract disorders, often combined with incontinence. As described in European Society for Pediatric Urology (ESPU) and Children and the International Children's Continence Society (ICCS), urotherapy has proven to be a successful treatment for children with functional incontinence and is increasingly considered the gold standard in the treatment of functional bladder and bowel problems. It is a combination of cognitive-behavioural and physical training, typically provided by urotherapists.
The urotherapist has a background in nursing, psychology, pedagogy or physiotherapy.
The urotherapist assesses, counsels and trains children with functional urinary and bowel problems.
Knowledge of normal bladder development and bladder control is essential for interpreting and treating abnormal bladder behaviour in children. Knowledge of bowel and rectum controle, constipation, its causes and treatment is also required.
A urotherapist needs specific skills to analyse and, where possible, resolve, prevent or reduce the need for care, and to select and implement appropriate (practice and evidence-based) interventions.
This seven-day course covers the medical and behavioural aspects and urotherapeutic management of children with functional problems of urination and defecation.
The following topics will be covered
- Anatomy and physiology of the urinary tract and bowel.
- Diagnosis and management of functional urinary and bowel dysfunction
- Medical aspects of functional bladder and bowel dysfunction
- Urotherapeutic diagnosis and treatment.
- Medical management of constipation, urinary tract infections and overactive bladder
- The young child, toilet training.
- Recognizing psychological issues
- Urotherapy and the behavioral aspects of treatment.
- Diagnosis and treatment of bedwetting.
- Invasive medical assessment - treatment for bladder and bowel dysfunction
- Professionalization and Science
Upon successful completion of the course, the professional will be able to fulfil the following roles
- Practitioner: in the field of medical diagnosis and urotherapeutic treatment of functional urinary and bowel problems in children;
- Organizer/coordinator: efficient, needs-based care from the child's perspective, taking into account the developmental stage.
- Professional and Quality Enhancer: managing, promoting and maintaining competence in urotherapy.
This course has been developed in close collaboration with the Urotherapy Department of the Wilhelmina Children's Hospital in Utrecht, University Medical Centre, The Netherlands.
Learning Objectives General
Learning objectives Urotherapy course
A urotherapist needs specific competencies to analyze and where possible resolve, prevent or reduce the demand for care and be able to select and implement the appropriate (practice- and evidence-based) interventions.
This seven-day course covers the medical, behavioral and urotherapeutic treatment of children with functional micturition and defecation problems.
Upon completion, the participant will have achieved the following final qualifications:
Basic knowledge regarding
- The anatomy and physiology of urinary tract and intestines.
- Diagnosis and treatment of functional micturition and defecation problems;
- The medical aspects
- The urotherapeutic diagnosis and treatment.
- Drug treatment constipation, urinary tract infections and overactive bladder;
- Urotherapy and the behavioral aspects of treatment
- Psychological aspects of incontinence
- Bedwetting, diagnosis and treatment.
- Additional medical examination
- Clinical decision-making
- The role of the urotherapist and the organization.
- Professionalization, knowledge and science
Upon successful completion of the training, the participant will be able to shape and substantiate the following roles, namely the role of:
- Healthcare provider: the field of medical diagnosis and urotherapeutic treatment of functional micturition and bowel problems in children;
- Organizer/coordinator: the area of efficient, demand-oriented care from the perspective the child, taking into account developmental stage.
- Professional and quality promoter: handling, promoting and maintaining professional competence in the field of urotherapy
The participant will acquire the following basic skills during the course and will be able to :
- Gain comprehensive knowledge of lower urinary tract dysfunction and constipation in children to improve the quality of care and clinical outcomes.
- Develop skills to adequately assess and interpret information obtained from the history and examination of children with bladder and defecation problems.
- Learn to make accurate (differential) diagnoses based on the child's history and medical records.
- Acquire the ability to make informed decisions about initiating urotherapeutic treatment
- Apply various elements of urotherapy, including standard urotherapy and specialized techniques such as biofeedback training, neuromodulation, and clean intermittent catheterization (CIC).
- Apply various treatment options of treating children with enuresis
- Apply communication techniques to build a therapeutic relationship between the parent, child, and therapist based on trust and respect.
- Provide empathetic psycho-education and instructions to parents and children regarding the causes and treatments of their conditions.
- Recognize and counsel parents and children regarding psychological symptoms and disorders
- Implement behavioral therapy techniques to coach and counsel the child effectively.
- Guide and motivate children and their parents throughout the treatment and training process, ensuring active participation and adherence to the treatment plan.
- Understand evidence based practice and contribute to the development of scientific expertise in the field of urotherapy.
Assessment
Assessment consists of a written report (3000 words maximum).
The written report is based on one or two case studies from one's own professional practice. The basis for this is formed according to the 6 steps of clinical reasoning
- Orientation: Ask the child or young person what their help request is and complete the tool together.What is really important to him/her? Would he/she want to change something? What do you need to achieve your goal?
- Clinical problem statement: Formulate a diagnosis/subdiagnosis based on the anamnesis
- Additional examination: support the diagnosis using the bladder and bowel diaries and if possible flowmetry measurement and ultrasound/bladder scan
- Policy: Formulate - based on current best evidence, professional knowledge of the urotherapeuticurotherapist and the value(s) and preference of the child and environment - a treatment plan, substantiate this from the literature
Describe how to explain normal bladder/bowel function and dysfunction to the child and parents and instructions for treatment to parents and the child.
Explain which urotherapeutic elements will be emphasized depending on the (sub)diagnosis and which behavioral therapeutic techniques are appropriate. - Treatment process : describe the course of treatment, what went well, what are the pitfalls for the child/parents, give concrete examples of how you motivated and coached the child.
If treatment is not successful describe what the most obvious cause is and what your next steps are. - Evaluate: your evaluation of care and reflection on your clinical reasoning. Reflect on your own actions and evaluate with a colleague or your work supervisor.
Contact
This email address is being protected from spambots. You need JavaScript enabled to view it., course coordinator
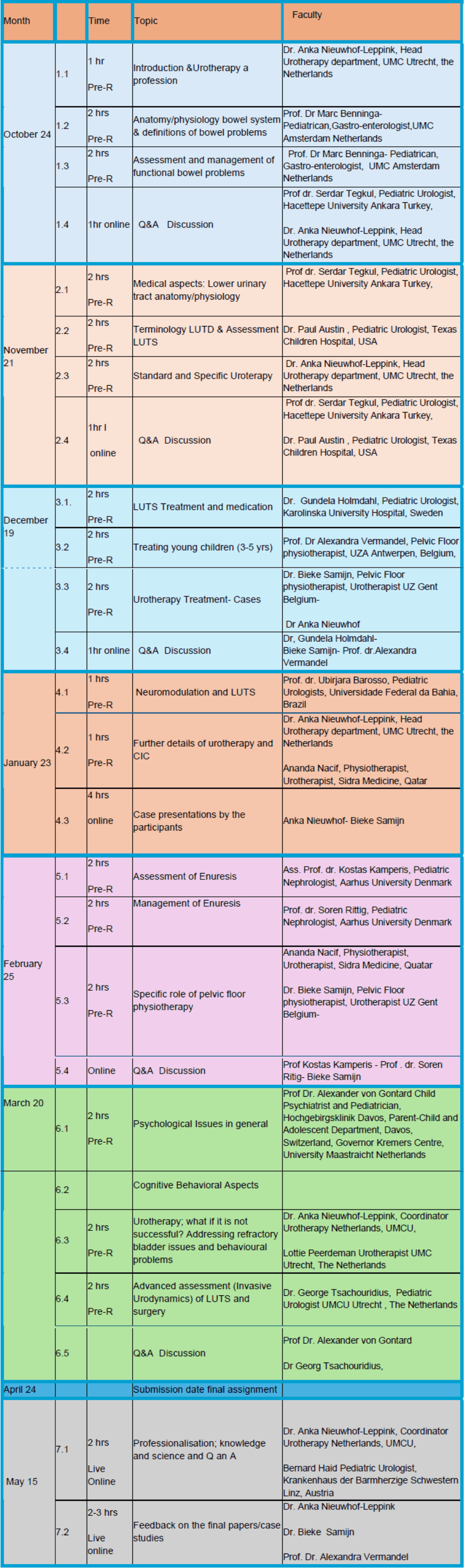
Program overview