
309
19–22 APRIL, 2017, BARCELONA, SPAIN
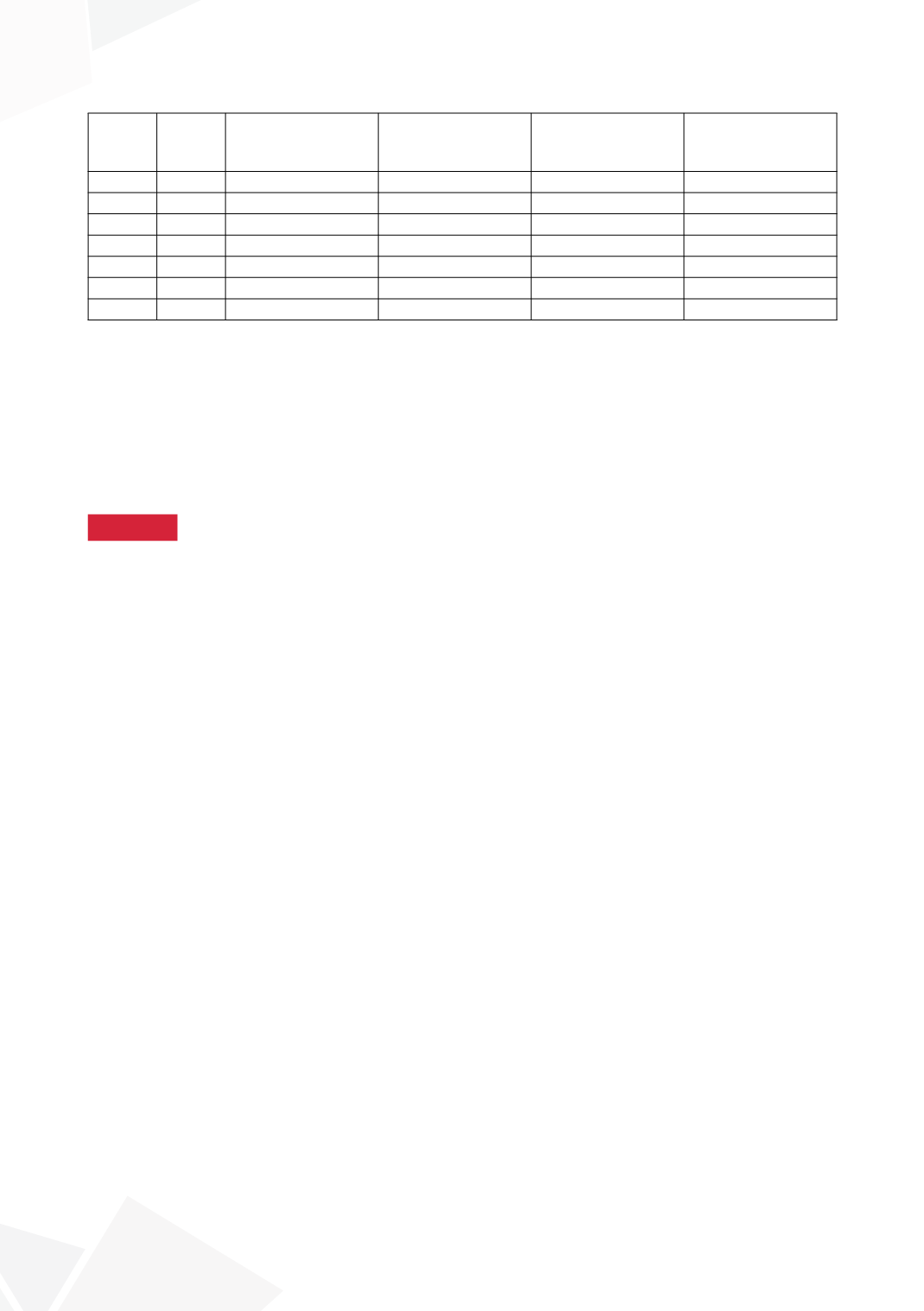
Patient
Age EBC for age in ml
Baseline MBC in ml
(EBC in %)
At 12 wks PTNS
MBC in ml (EBC
in %)
% Increase
1
9
300
150(50%)
250(83%)
+23%
2
8
270
100(37%)
200(74%)
+37%
3
9
300
100(33%)
250(83%)
+50%
4
8
270
200(74%)
300(111%)
+37%
5
12
390
190(48%)
290(74%)
+26%
6
9
300
175(58%)
300(100%)
+42%
7
10
330
220(66%)
295(89%)
+23%
Needle puncture was not experienced as traumatic. Peers contact had additional therapeutic value.
The optimal maintenance schedule is to be studied.
CONCLUSIONS
Preliminary results of PTNS in children with therapy-resistant OAB are promising. Bladdercapacity
increased and overall incontinence episodes decreased. Further study results are presented
in 2018.
10:10–10:20
S1-6 (LO)
THE EFFECT OF BIOFEEDBACKTRAINING ON STACCATO
AND INTERRUPTED UROFLOWS OF CHILDREN
WITH DYSFUNCTIONAL VOIDING
Nienke IDSARDI
1
, Anka NIEUWHOF-LEPPINK
2
, Jorinde KORTENBOUT
3
, Bennie TEN
HAKEN
4
, Pieter DIK
5
and Aart KLIJN
6
1) University Children’s Hospital UMC Utrecht/ University of Twente, Pediatric urology/Technical Medicine, Westergeest,
NETHERLANDS - 2) University Children’s Hospitals UMC Utrecht and AMC Amsterdam, Pediatric Urology,
Utrecht, NETHERLANDS - 3) University of Twente, Technical Medicine, Enschede, NETHERLANDS - 4) Univeristy
of Twente, Faculty Science and Technology Dept. of Neuroimaging (NIM), Enschede, NETHERLANDS - 5) University
Children’s Hospitals UMC Utrecht and AMC Amsterdam, Pediatric Urology, Utrecht, NETHERLANDS - 6) University
Children’s Hospitals UMC Utrecht and AMC Amsterdam, Pediatric Urology, Utrecht, NETHERLANDS
PURPOSE
The talking toilet (TT) is a home uroflowmeter designed for children that gives objective scores to
flows and produces immediate spoken feedback to the child. Analysis of the TT uroflow curves of
children with dysfunctional voiding, showed that, in a tertiary centre setting with patients, refractory
to earlier treatment in a secondary setting, the biofeedback training produced no improvement in
uroflow curves. Therefore, we did a study to compare results in a secondary, general pediatrician
setting, and our tertiary situation.
MATERIAL AND METHODS
Sixty eight children with dysfunctional voiding, aged 5-16, were included in 3 groups: 25 children
had standard outpatient training with addition of the TT, 13 children had standard outpatient training
in a tertiary center, 30 children had standard outpatient training in a secondary center. The uroflows
have been analyzed by professionals involved in urotherapy and pediatric urology and have also
been analyzed using the software of the TT. Linear mixed models analyzed whether time has an
effect on the scores.
RESULTS
Differences exist between the improvement of urowflows of these 3 groups. Uroflowcurves of third
line referrals improve less or do not improve, compared to secondary settings.









