
108
28
TH
CONGRESS OF THE ESPU
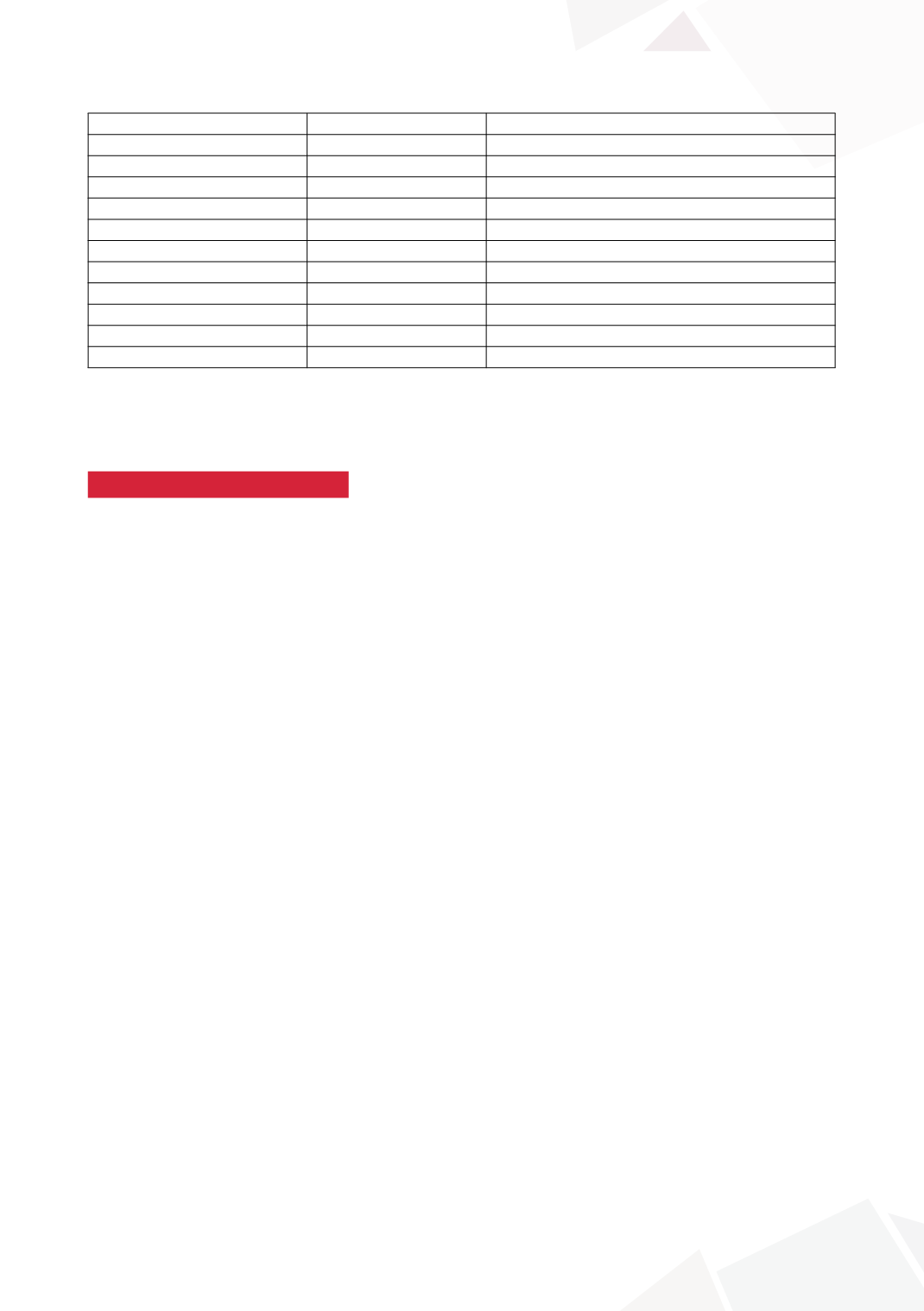
Open repair
Laparoscopic high ligation
Patients No.
22
55
Age
29 month (19-65)
37 month (18-136)
No. side/total No. (%)
Rt
12 (54.5)
34 (61.8)
Lt
9 (40.9)
16 (29)
Both
1 (4.5)
17 (30.8)
Operative time
25 mins (15-35)
14 mins (5-28)
Hospital stay
1 d
1 d
f/u duration
16 month (6-26)
14 month (2-25)
Recurrence
0
2
Complication
7
0
CONCLUSIONS
It was not necessary to remove the hydrocele sac in pediatric hydrocele. The high ligation of PPV is
only an effective procedure for pediatric hydroceles.
S9-13 (P without presentation)
ABDOMINAL IMAGING IS UNNECESSARY
IN THE EVALUATION OF THE PEDIATRIC VARICOCELE
Martin KAEFER
1
, Konrad SZYMANSKI
2
, Benjamin WHITTAM
2
, Rosalia MISSERI
2
,
Katherine HUBERT
2
, Richard RINK
2
and Mark CAIN
2
1) Riley Hospital for Children, Urology, Indianapolis, USA - 2) Riley Hospital for Children, Pediatric Urology, Indianapolis,
USA
PURPOSE
The evaluation and treatment of the pediatric varicocele remains controversial. The paradigm for
management has often been based on the strategy used for adults. It has been commonly taught
that an adult, who presents with sudden onset varicocele, bilateral varicoceles, or unilateral right-
sided varicocele, should be evaluated for an intra-abdominal process that could be causing external
compression of the gonadal vein. We sought to determine the value of this practice in the pediatric
population.
MATERIAL AND METHODS
A retrospective chart review was made of all individuals presenting to our pediatric unit between
1999 and 2012 with the diagnosis of a varicocele. All patients who underwent abdominal imaging
as a part of their evaluation were included. Patients older than 18 years were excluded. Age at pres-
entation, laterality, grade, calculated testicular size and mode of abdominal imaging were recorded.
RESULTS
Eighty-eight of 600 boys presenting with a varicocele underwent abdominal imaging (15%).
Indications included left sided varicocele (48), bilateral varicocele (11), right-sided varicocele (5),
and recurrent varicocele (2). Twenty-two patients underwent abdominal imaging due to concern
over other systemic complaints (for example abdominal discomfort). A total of 98 imaging studies
were obtained (94 ultrasounds, 3 CTs, 1 MRI). In no case did the abdominal imaging reveal any in-
traperitoneal or retroperinoeal process causing compression of the gonadal vasculature. Incidental
focal nodular hyperplasia of the liver was identified in a single patient with a left sided varicocele, but
the involvement was well away from the renal hilum and gonadal vein.
CONCLUSIONS
Although abdominal imaging for rapid onset left, bilateral, or unilateral right-sided varicoceles has
been proposed in adults, the value of this screening is of negligible value in the pediatric population.









