
106
28
TH
CONGRESS OF THE ESPU
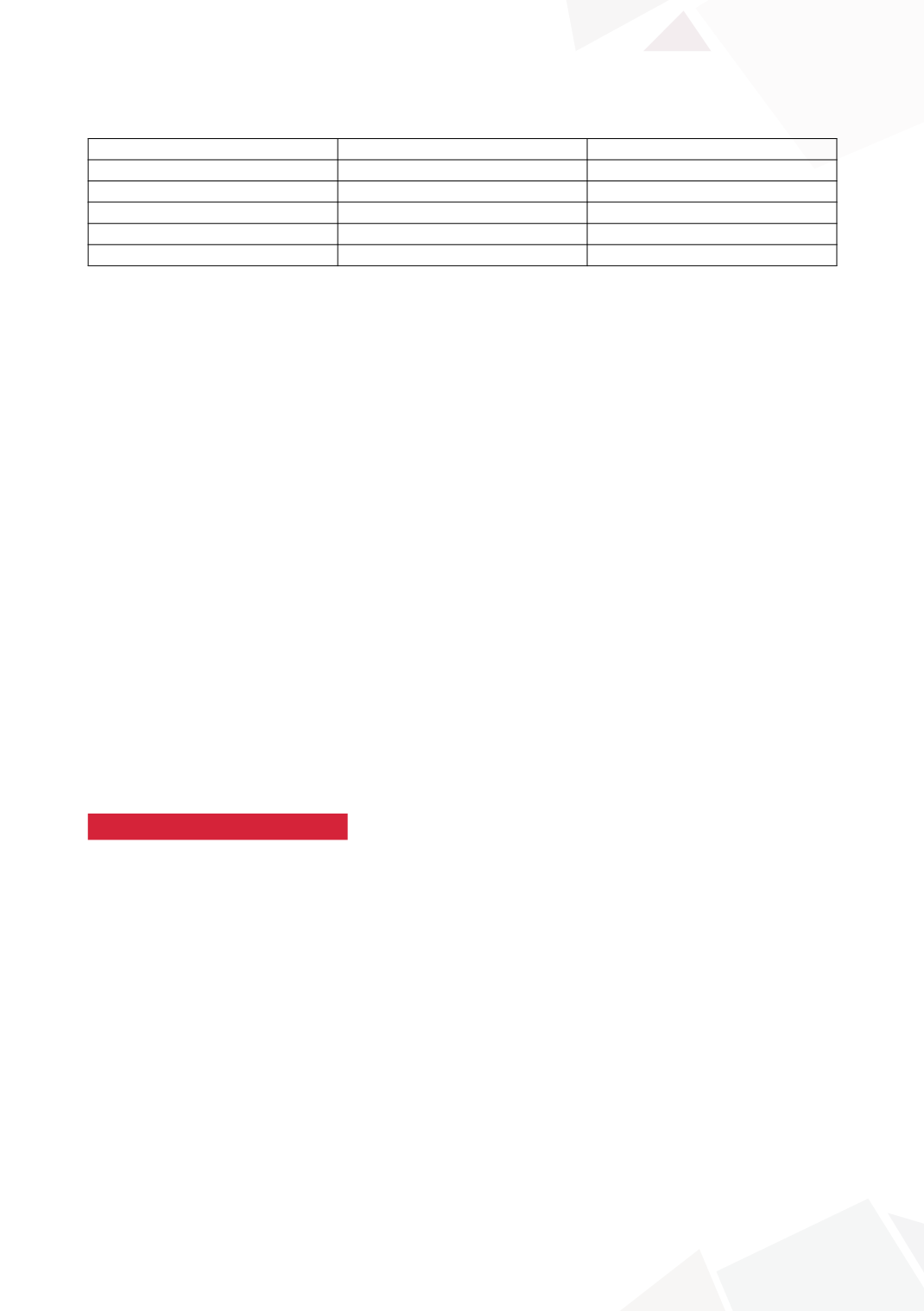
Top-5 referrers:
Specialty
Referral-number
Referrals-with-imaging
General-Practitioner
141
21%
Adult-Urology
134
63%
Paediatrics
95
39%
Endocrinology
20
30%
Adult-Surgery
11
72%
USS Reports:
209 testes “abnormal” - Incorrect report in 28% based on operation undertaken
A) “Absent/Not-seen” - 59
26 (44%) false negative: 13 palpable (single-stage-orchidopexy), 13 intra-abdominal
(laparoscopic-Fowler-Stevens-orchidopexy)
B) “Undescended”- 150
33 (22%) false positive location:
21 reported “intra-abdominal” but 4 palpable (single-stage-orchidopexy), 2 intra-abdominal testicu-
lar remnants which were excised.
129 reported “groin-position” but 17 were intra-abdominal requiring laparoscopy, 8 descended on
clinical-examination and 2 testicular-remnants.
US for impalpable testis (4) suggesting a favourable groin-location lead to unsuccessful exploration
at the referring-centre. This resulted in testicular loss(1), revision open-orchidopexy(2) and revision
laparoscopic two-stage operation(1).
MRI
5 MRI scans for impalpable testis in four patients identified only one testis. This was reported as
intra-abdominal but was in fact palpable and underwent single-stage-orchidopexy. Laparoscopy
confirmed absent testis in the remaining three.
CONCLUSIONS
Pre-referral imaging for UDT is common and is likely grossly underestimated in this study. The
USS-reported abnormal location of the testis when “seen” was inaccurate in 22% and, if used as
the basis for surgical-approach, can lead to morbidity. The psychological impact of imaging remains
un-quantified. Educational programmes could reduce resource wastage, financial expenditure and
most importantly provide correct and timely management.
S9-11 (P without presentation)
ORCHIDOPEXY IN INFANTS WITH PRADER-WILLI
SYNDROME: A 12-YEAR SINGLE CENTRE EXPERIENCE
Audrie LIM
1
, Alexander MACDONALD
1
, Nicola BRIDGES
2
and Marie-Klaire FARRUGIA
1
1) Chelsea and Westminster NHS Foundation Trust, Paediatric Surgery and Urology, London, UNITED KINGDOM -
2) Chelsea and Westminster NHS Foundation Trust, Paediatric Endocrinology, London, UNITED KINGDOM
PURPOSE
A variety of anatomical and physiological factors make the surgical and anaesthetic management of
cryptorchidism in Prader-Willi syndrome (PWS) challenging. Optimal age for orchidopexy in these
invariably infertile infants remains unclear. We reviewed our 12-year single-centre experience to
establish our success rate and determine optimal age for orchidopexy.
MATERIAL AND METHODS
14 infants with PWS referred for orchidopexy were identified from a prospectively maintained
database. Case records retrospectively reviewed by 2 independent reviewers.









