
163
19–22 APRIL, 2017, BARCELONA, SPAIN
RESULTS
The overall complications rate was significantly higher after RPN (21/50- 42%) than after LPN (10/52-
19%) [χ2 = 0.05 ]. In LPN group, complications (4 urinomas, 2 symptomatic refluxing distal ureteral
stumps (RDUS) with recurrent UTIs and 4 urinary leakages) were managed conservatively. In RPN
group, complications (6 urinomas, 8 symptomatic RDUS, 6 peritoneal perforations and 1 opening
of remaining calyxes) required a re-operation in 2 patients. Operative time (LPN:166.2 minutes vs
RPN: 255 minutes; p<.001) and hospitalization (LPN: 3.5 days vs RPN: 4.1 days; p<.001) were
significantly shorter in LPN group. No post-operative loss of renal function was reported in both the
groups.
CONCLUSIONS
Our results demonstrated that RPN remains a technically demanding procedure with a significantly
higher complications and re-operation rate compared to LPN, also in expert hands. LPN seems to
be faster, safer and technically easier compared to RPN due to a larger operative chamber avail-
able, a good overall exposure of the anatomy of the kidney and the possibility to perform a complete
ureterectomy in refluxing systems, avoiding to leave a refluxing ureteric stump.
11:03–11:06
S15-7 (PP)
PERI-OPERATIVE OUTCOMES OF LAPAROSCOPIC
AND OPEN ADRENALECTOMIES – 28 YEAR’S EXPERIENCE
Siam Wee SIM, Pankaj MISHRA, Abraham CHERIAN and Imran MUSTHAQ
Great Ormond Street Hospital for Children, NHS Foundation Trust, Department of Paediatric Urology, Singapore,
SINGAPORE
PURPOSE
We compare perioperative outcomes of laparoscopic and open procedures in 57 adrenalectomies
with emphasis on complete resection.
MATERIAL AND METHODS
Retrospective review of all the primary adrenalectomies from April 1988 to April 2016, excluding
neuroblastoma and redo surgeries. The outcomes were compared with Fisher’s Exact Test.
RESULTS
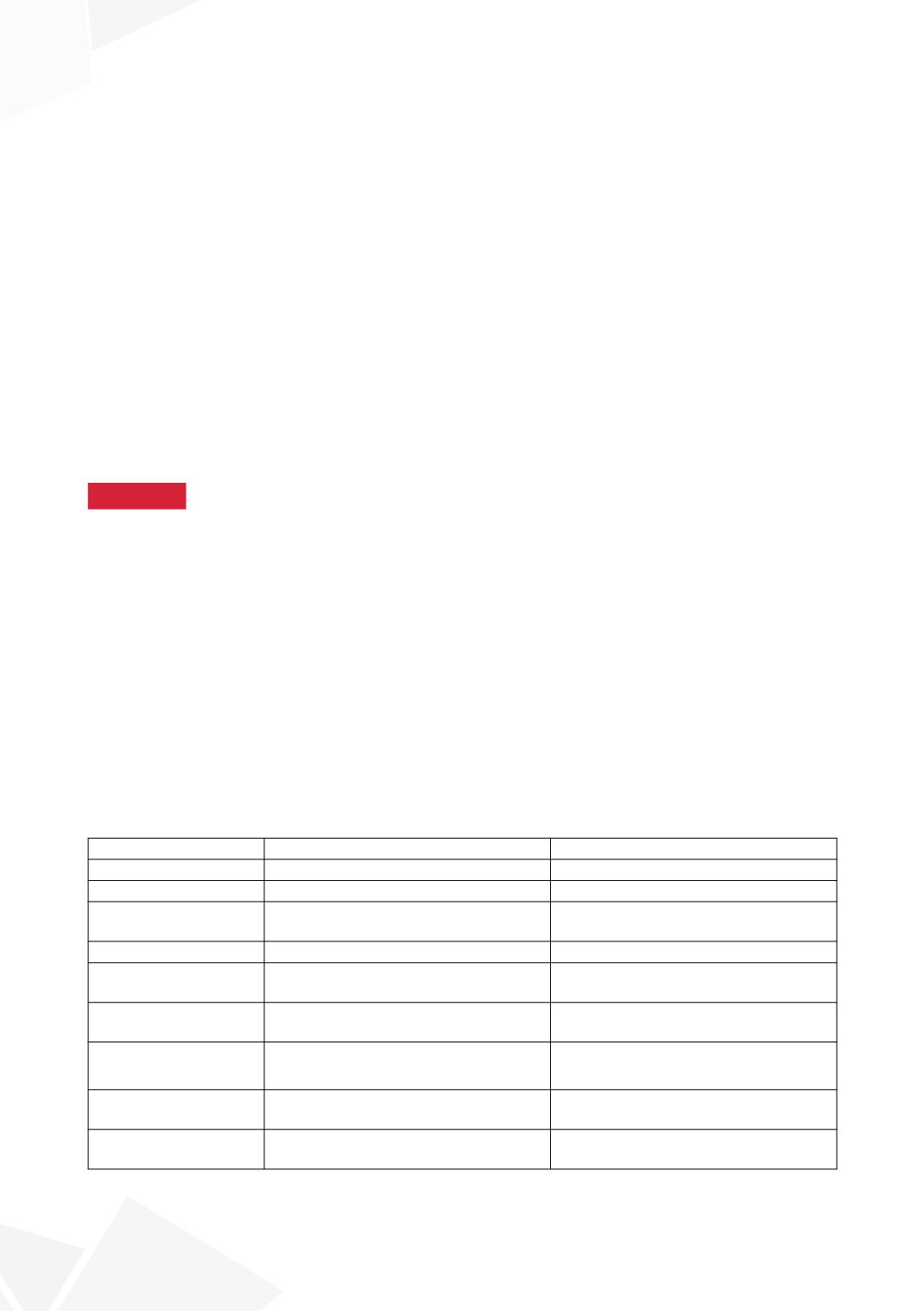
Approach
Laparoscopic
Open
Number
28(21Retro/7trans)
29
Sex
10males, 15females
16males, 12females
Age
(median, months)
64
44
Side
7left,7right,7bilateral
9left,18right,1bilateral
Surgery time
(median,minutes)
122(35-340)
170(60-630)
Weight
(median,grams)
15.6(0.5 – 72.5)
80.0(4.0-1566.0)
Volume
(median,cm
3
)
30(1-168)
103(2-2243)
Operative capsular
breach
2(Patient 1&2)
5
Microscopic margins
positive
1(patient 2)
4









